|
Now, more than ever, there is an abundance of misinformation circulating about the safety and benefits of exercising during pregnancy. It can be incredibly confusing and disheartening when you are simply trying to do what is best for you and your baby, and every source you consult for advice contradicts the previous one. Let's clarify one thing right from the start: if you are healthy and experiencing a "normal" pregnancy, it is perfectly safe to continue or begin exercising. To set your mind at ease, ACOG states that "physical activity does not increase your risk of miscarriage, low birth weight, or early delivery." As always, it is important to discuss your exercise plan with your obstetrician during the early stages of pregnancy. Now that we have covered the basics, let's delve into the specifics of exercising during pregnancy. What makes exercise a potential risk factor? What are the benefits, and what do experts recommend? What Conditions Make Exercise During Pregnancy a Risk Factor? There are certain conditions and pregnancy complications that require special attention, and you should ALWAYS consult with your obstetrician before engaging in any physical activity. In such cases, they will likely recommend a more sedentary lifestyle throughout your pregnancy. The American College of Obstetricians and Gynecologists has provided a list of these conditions, which include:
What are the Benefits of Exercising During Pregnancy Exercising regularly throughout your pregnancy provides a wealth of benefits, from pain relief to reducing the risk of certain pregnancy complications. Understanding these benefits is crucial to appreciating the importance of staying active for both you and your baby. Pain Relief: Regular exercise during pregnancy is particularly effective at alleviating back pain. Exercise strengthens the muscles in the back, reducing weakness and soreness, while increasing blood flow to the area, making it feel less stiff. Constipation Relief: Many of our pregnant patients confide in us about their frustrating, irregular bowel movements. Exercise is a simple and effective way to get your digestive tract moving regularly. It decreases the time it takes for food to travel through the large intestine, reducing the amount of water your body absorbs from stool, which helps to prevent hard, dry stool that's harder to pass. Gestational Diabetes: According to the Centers for Disease Control and Prevention (CDC), between 2% and 10% of pregnancies are affected by gestational diabetes. This type of diabetes is caused by hormones secreted by the placenta to support the pregnancy, making the body's cells temporarily resistant to insulin and resulting in high blood glucose levels. Exercise helps combat this by reducing blood glucose levels through increased glucose consumption by muscle cells. Exercise can also make muscle cells more sensitive to insulin, meaning they continue to consume glucose after the workout is over. Preeclampsia: Indicators of preeclampsia include high blood pressure, high protein levels in urine, and other signs of organ damage, often beginning around or after 20 weeks of pregnancy in people whose blood pressure was previously in the normal range. According to a recent study, exercise interventions during pregnancy reduced the risk of pregnancy-induced hypertension and preeclampsia by 39% and 41%, respectively, according to the Mayo Clinic. What’s Recommended Now that we understand why exercise is crucial during pregnancy, it's important to determine the most beneficial types and amounts of exercise. According to ACOG, pregnant women should aim for at least 150 minutes of "moderate-intensity aerobic activity" per week. To elaborate, moderate intensity refers to an activity that makes you break a sweat and raises your heart rate, allowing you to hold a conversation but not sing. Aerobic activity involves rhythmic movement of the large muscles in your body, such as walking, running, cycling, and dancing. If you weren't physically active before pregnancy, it's advisable to begin with low-intensity exercises and gradually increase your activity level. Conversely, if you were very active before becoming pregnant, you can continue with your usual routine, subject to your obstetrician's approval. While most of the physical activities you did before pregnancy are safe to continue, there are exceptions to the rule. Contact sports that may cause abdominal injury and sports that pose a risk of falling, such as horseback riding and skiing, should be avoided. Also, avoid hot yoga or hot Pilates, as they may lead to dehydration and overheating. The Bottom Line In conclusion, exercise is an essential component of a healthy pregnancy. It provides numerous benefits, from pain relief to reducing the risk of pregnancy complications like gestational diabetes and preeclampsia. However, as with any medical advice, it's crucial to consult with your obstetrician before starting or continuing any exercise routine. Your doctor can help you develop a safe and effective exercise plan that meets your specific needs and circumstances. Remember, every pregnancy is different, and what works for one person may not work for another. By working closely with your healthcare provider and staying active, you can help ensure a healthy pregnancy for you and your baby. Davenport MH, Ruchat S-M, Poitras VJ, Jaramillo Garcia A, Gray CE, Barrowman N, et al. Prenatal exercise for the prevention of gestational diabetes mellitus and hypertensive disorders of pregnancy: a systematic review and meta-analysis. Br J Sports Med. 2018;52(21):1367–75.
https://www.acog.org/womens-health/faqs/exercise-during-pregnancy https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy-and-exercise/art-20046896 https://www.cdc.gov/diabetes/basics/gestational.html#:~:text=Gestational%20diabetes%20is%20a%20type,pregnancy%20and%20a%20healthy%20baby.
0 Comments
Pregnancy is a time of immense change, both physically and emotionally. As your body prepares to bring a new life into the world, your bones, joints, ligaments, and muscles all work together to create a safe and nurturing environment for your baby. But all these changes can also cause discomfort, pain, and other symptoms that can make this time challenging. Many pregnant folks assume that these symptoms are just a normal part of the pregnancy experience, something that can’t be avoided, but that's far from the truth. We hear each and every day, "I was told this is just a normal part of having a baby, that it happens to everyone." We're here to break this stigma and assure you that just because symptoms are common doesn't mean they're normal and you don't have to just "learn to live with it." As pelvic floor specialists, we believe that everyone deserves a happy, healthy, and active pregnancy and postpartum experience. Pelvic floor physical therapy can help you achieve that by addressing the various symptoms that arise during pregnancy, labor, and postpartum, teaching you techniques for remaining active, and providing valuable, personalized insight on how your body reacts to certain birthing positions. Pregnancy The earlier you start pelvic floor PT during pregnancy, the better. By starting early, we can ensure that your body is well-prepared for what's to come and can help mitigate any symptoms that may arise. We can also provide you with education and strategies to help you navigate this time successfully. Physical Exercise: Pelvic floor PT can guide you on how to exercise safely and effectively during pregnancy, so you can have an active pregnancy as you desire. We'll teach you proper breathing techniques, posturing techniques, and exercises that have been proven effective time and time again. Pain: It's common to experience lower back, hip, pelvic, or pubic pain during pregnancy. Pelvic floor PT can help relieve this pain by using a combination of treatment techniques, teaching you how to "turn on and off" the appropriate muscles, and providing knowledge on how to manage pain if it flares up in the future. Coordination: To prepare for labor, it's essential to have a thorough understanding of how to contract, relax, and bear down the pelvic floor muscles effectively. Consulting with a Pelvic PT can help improve the motor control of these muscles and increase awareness of their function Labor Prep: Pelvic floor PT can also optimize the labor process. We'll teach you techniques to aid in your labor experience, including insight on effective birthing positions, relaxation strategies, and perineum stretching that your support system can perform. Postpartum
Postpartum can be a confusing time, and it's normal to feel overwhelmed and unsure of what to do. At Restoration Health Collective, we provide essential guidance and support during this time when you may need it most. Pelvic floor PT can help you not only get rid of any lingering symptoms but also get you feeling better than you ever have before. Our goal is to not just return you to your prior level of function, but to help you feel even better than you did before. For all the moms, moms-to-be, or support systems for mothers, it's important to remember that you don't have to suffer from these symptoms forever. Working with a skilled, pelvic floor physical therapist who provides individualized care can relieve you of your symptoms, get you back to feeling your best, and significantly improve your overall quality of life. Whether you're thinking of becoming pregnant, pregnant, or postpartum, pelvic floor PT can make the difference between just managing symptoms and thriving. If you're interested in booking an appointment or have questions about pelvic floor PT, call our office. We'd love to help guide you on the path to relief. Urinary incontinence and dysfunction can be a frustrating and embarrassing experience for so many. We've seen even the most confident, capable individuals left feeling hopeless and like they have nowhere to turn all because of leaking, urgency, and frequency. However, it's essential to know that you're not alone and that there are solutions to help alleviate your symptoms. Our goal is to help crush the stigma surrounding urinary incontinence and dysfunction and provide you with hope and relief.
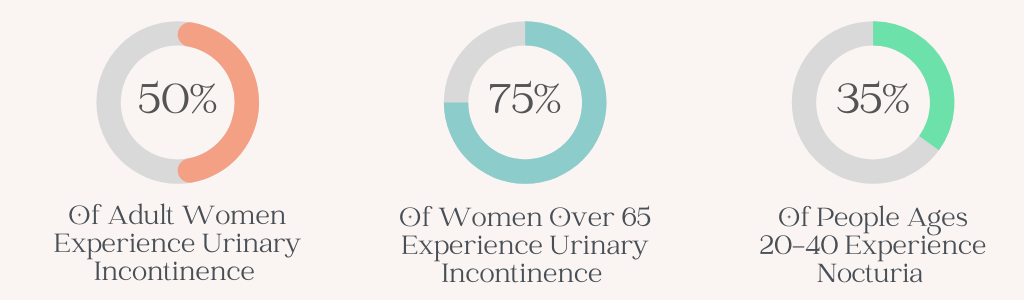
If you're looking for tips and tricks to find relief before booking an appointment with a pelvic floor PT office in Baton Rouge, keep reading. In this blog post, we'll provide you with our top products and techniques to help you hold on until you find true relief. Please note that these tips are temporary Band-Aids, and true relief comes when you address the root cause of your symptoms. Do you find yourself constantly making excuses for your frequent bathroom breaks or laughing off the occasional leakage? Catch yourself saying, “Nooo don’t make me laugh I’m going to pee my pants”? You're not alone. Millions of people in the United States suffer from bladder dysfunction, yet so many of us simply brush it off as a normal part of life. https://www.urineincontinence.com.au/other/frequent-urination-night-ornocturia#:~:text=Nocturia%20is%20a%20very%20common,once%20or%20more%20at%20night https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/is-urine-incontinence-normal-for-women The truth is, bladder dysfunction is not something to be taken lightly. It can significantly impact your quality of life, causing embarrassment and discomfort, and even leading to social isolation. In this blog post, we'll be shedding some light on this common condition, and helping you to spot the signs of bladder dysfunction in yourself. Types of Bladder Dysfunction There are several types of bladder dysfunction, each with their own unique symptoms and causes. Here are some of the most common: Stress Incontinence: This occurs when urine leaks out during activities such as laughing, coughing, sneezing, bending, or lifting. This is what’s happening when your mom, aunt, or grandma say, “Every time I sneeze, I pee a little!”. It's caused by a mechanical issue where the pressure in your bladder is stronger than the pressure in your pelvic floor. . Stress incontinence can also be due to a timing issue, if your pelvic floor squeezes after the pressure in your bladder increases, you’ll still leak no matter how fit your pelvic floor is. Pelvic floor physical therapy can be effective in treating this issue by strengthening the pelvic floor muscles whether that means lengthening the muscle or working to make it shorter. This will help you to stay dry no matter how funny your friend is and regardless of how intense your workout will be that day. https://phoenixpt.com/statistics/#:~:text=Urinary%20Incontinence%20affects%20200%20million%20people%20worldwide.&text=One%20in%20four%20women%20over,episodes%20of%20leaking%20urine%20involuntarily.&text=On%20average%2C%20women%20wait%206.5,bladder%20control%20problem(s). Urge Incontinence: This is the classic, key in the door scenario, you’re almost to the bathroom but you just don’t quite make it. You’ll often experience a sudden, intense urge to urinate and are unable to hold it long enough to reach the restroom. This is usually caused by an overactive bladder or irritation in the pelvic floor muscles. Mixed Incontinence: This is a combination of stress and urge incontinence, where you experience symptoms of both conditions simultaneously. Urgency: This is when your brain is unable to differentiate between the different levels of urgency being relayed from the bladder until it’s too late. Think back to our previous blog post when we discussed the three levels, we want you to be able to hear the bladder’s whispers, not just the shouts. Frequency: If you find yourself going to the bathroom more than every 3-5 hours, this may be a sign of bladder dysfunction. Your bladder should be able to hold urine for several hours before you feel the urge to go again. If you catch yourself running to the bathroom every 45 minutes but you “drink a lot of water,” that’s still a problem driven by your pelvic floor. It’s not that your bladder is small, it’s because it’s not flexible enough. Emptying Troubles: If you encounter challenges initiating or ending your urine flow or experience a weak and inconsistent stream with interruptions or dribbling, it may indicate issues with your pelvic floor muscles. As we previously discussed in a blog post, your bladder and pelvic floor muscles engage in a "red light/green light" game. If they are not working in harmony, this can result in delayed start of stream, difficulty emptying, and other related issues. Discomfort or Burning: If you experience burning or discomfort during urination, it could be due to an infection or issues with the pelvic floor muscles. Frequent UTIs with negative urine cultures may also indicate a problem with the muscles. We work with physicians to help get to the root of the issue, whether that due to the muscle or an infection. Nighttime Urination: We often hear people say “Oh my gosh I have to pee 3-4 times before I can actually fall asleep cause it feels like there’s still urine left in my bladder,” or “I wake up every night to pee but I always drink a lot of water before bed.” Waking up multiple times to urinate or feeling like there is still urine in your bladder after urinating are both signs of bladder dysfunction.
Treatment for Bladder Dysfunction: Pelvic floor physical therapy is often an effective treatment for bladder dysfunction. Through strengthening exercises and relaxation techniques, your pelvic floor muscles can be trained to function properly and alleviate symptoms. In addition, lifestyle changes such as reducing caffeine and alcohol intake, and maintaining a healthy diet can also improve bladder function. Don't let bladder dysfunction control your life. Seek help from a pelvic floor physical therapist today to address the issue and improve your quality of life. Urine Good Hands : Understanding the Bladder, How it Works, & The Role of the Pelvic Floor3/22/2023 Hey there! In previous blog posts, we've talked about the importance of the pelvic floor and how it affects our bodies. Today, we're going to dive into the bladder and how it works when everything is functioning properly. Let's think of the bladder like a balloon. It's a flexible object that can expand and shrink, just like when you're trying to learn how to do a split. With practice and persistence, your leg becomes more and more flexible, and similarly, the bladder can adjust to its contents. The kidneys produce a drop of urine every ~14 seconds, which flows down the ureter and lands in the bladder. This cycle continues until the bladder is slowly filled. As it fills up, you'll start to feel a stretching sensation, just like when you're stretching any other part of your body. This is the point where your brain tells you that you need to go to the bathroom.
A Guide to the World of Laxatives, Stool Softeners, Enemas, and Supplements for Bowel HealthINTRO In our previous blogs, we discussed the importance of healthy bowel function, what is normal and what is not, and what happens when things go wrong including constipation & fecal incontinence. Today, we're diving deeper into the topic and exploring the worlds of laxatives, stool softeners, and enemas. With so much buzz around "gut health" and its various aspects, it's essential to understand these tools' proper use to maintain optimal digestive function. Join us as we navigate through the benefits, risks, and best practices of these bowel aids. Let's get started! LAXATIVES & STOOL SOFTENERS First, let’s talk about what we’re all probably the most familiar with, laxatives. The laxative industry is MASSIVE in the United States with an estimated $725 million spent annually. Yes, you read that right, $725 MILLION. This number is even more shocking when you realize that most people who take laxatives don’t actually need them and that their constipation woes would go away with an increase in fluid intake, adding fiber to their diet, moving their bodies more, and seeing a pelvic floor physical therapist. There are several different classifications of laxatives which include:
We always recommend consulting your doctor and pelvic floor physical therapist before taking any laxatives. ENEMAS Enemas are a procedure that involves the introduction of liquid into the rectum to promote bowel movement. They are commonly used to relieve constipation or to prepare for certain medical procedures such as a colonoscopy. Enemas can be useful in the context of pelvic floor dysfunction when constipation is a contributing factor. When stool sits in the rectum for prolonged periods, it can contribute to pelvic floor muscle tension and discomfort. Enemas can be a useful tool for promoting regular bowel movements and reducing pelvic floor muscle tension. However, there are potential risks associated with enemas, such as rectal bleeding, perforation of the rectum, and infection. It is important to follow proper instructions and consult with a healthcare professional, such as a pelvic floor physical therapist, before using an enema. A pelvic floor physical therapist can provide guidance on the safe and effective use of enemas and work with patients to develop a comprehensive bowel management plan that addresses their unique needs. IN CONCLUSION
Although laxatives and enemas can provide temporary relief for constipation and bowel dysfunction, it's essential to address the root cause of the problem for long-term improvement. Using these products without addressing the underlying issues may only provide temporary relief, and the symptoms are likely to recur. That's why we recommend seeking professional help to address the root cause of your symptoms. Pelvic Floor Physical Therapy is a highly effective treatment option for bowel dysfunction, including constipation, fecal incontinence, or a combination of the two. Our residency-trained, board-certified pelvic floor physical therapist can provide personalized care to help you overcome these issues and improve your quality of life. To learn more and book a complimentary phone consultation, simply click HERE or call our office at (225) 831-5140. Don't let bowel dysfunction control your life - take the first step towards relief today. Sources: https://www.verywellhealth.com/osmotic-laxatives-for-constipation-1944785 https://www.healthline.com/health/digestive-health/bulk-forming-laxatives#benefits https://www.everydayhealth.com/digestive-health/all-about-laxatives.aspx https://www.rxlist.com/how_do_lubricant_laxatives_work/drug-class.htm https://www.verywellhealth.com/osmotic-laxatives-for-constipation-1944785 https://www.mayoclinic.org/drugs-supplements/laxative-oral-route/description/drg-20070683#:~:text=Stimulants%E2%80%94Stimulant%20laxatives%2C%20also%20known,of%20laxative%20for%20self%2Dtreatment. https://www.verywellhealth.com/before-you-use-stool-softeners-1944786 Wait…That’s Not Normal?!
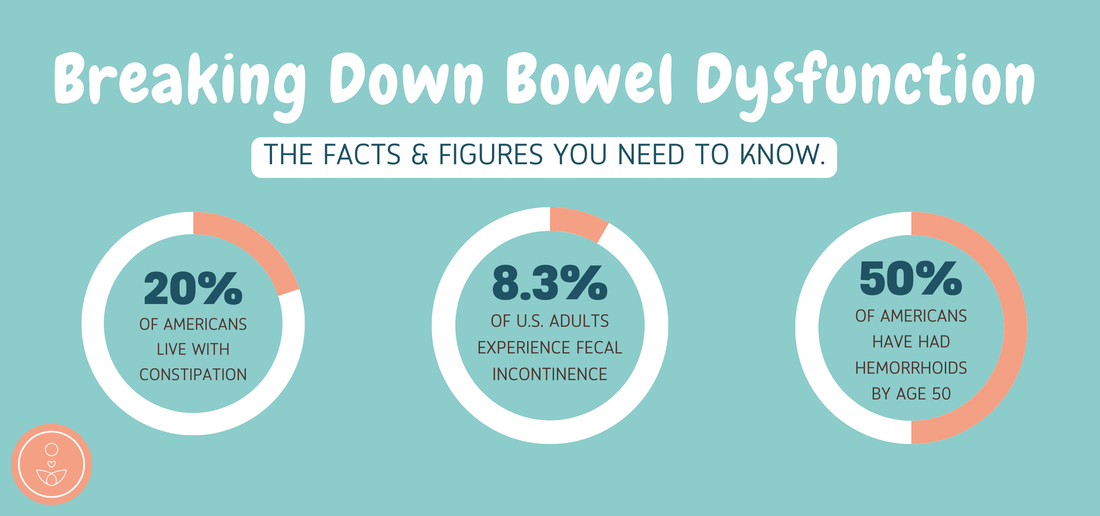
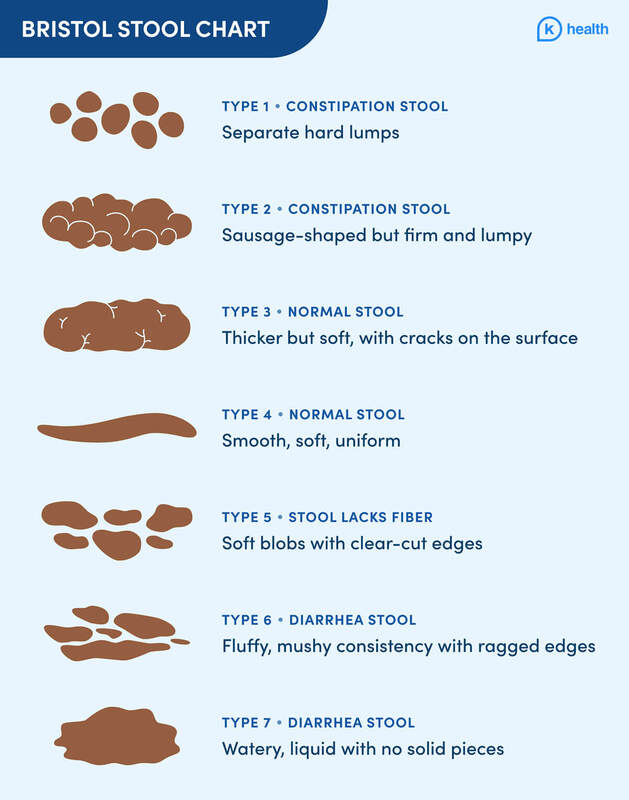
Now that we have a clear understanding of the bowels, how they function, and what’s considered “normal” when it comes to bowel movements (if you’re thinking “WAIT! What are they talking about?!” check out our last blog post for more information) it’s time to understand what’s NOT normal. There are symptoms that you might be experiencing without even realizing that they're symptoms because they've “always” been a part of your life or it happens to “everyone” in your family, or your mom told you “It’s just a part of getting older”. However, let's reiterate that just because it’s common, doesn't mean it’s normal! There is no reason for you to be struggling through your daily life with painful constipation, embarrassing fecal leakage, or gas that sneaks up on you. If you find yourself saying “This is totally me…” keep on reading! In this blog will be diving into the ins & outs of constipation, why you may be leaking stool, and the truth behind gas that slips out at the worst possible time. So, let’s get into it! Do you go days between bowel movements? Do you find yourself constantly wiping or experiencing discomfort during bowel movements? Do you feel like you've tried every fiber supplement, laxative, and stool softener on the market without any relief? If you've exhausted all the usual remedies without success, it may be time to consider the possibility of a pelvic floor problem. Our clinic specializes in helping people just like you achieve optimal bowel function and reclaim their quality of life. The good news is that you don't have to suffer in silence. As experts in pelvic floor physical therapy, we're here to help you get back to feeling your best. Understanding what's normal and what's not when it comes to bowel function is the first step towards a happier, healthier life. So, let's get started on this journey together. The Land of Misconceptions As pelvic floor physical therapists, we know that discussing bowel movements can be an uncomfortable topic for many people. However, understanding how your bowels work and what's normal is crucial to maintaining good health. Unfortunately, there are many misconceptions about bowel function that can lead to confusion and unnecessary discomfort, leaving many people struggling with bowel dysfunction without even realizing it's a problem. One common misconception is that certain symptoms are less valid simply because they have always been present. This couldn't be further from the truth. If you are experiencing discomfort or irregularity with your bowel movements, it's important to seek help and understand what is normal and what isn't. How Do The Bowels Work? When you eat, food travels through your digestive system, breaking down and absorbing nutrients along the way. However, the journey from your mouth to your rectum isn't a smooth ride - it's facilitated by rhythmic waves called peristalsis. Peristalsis is the involuntary movement of muscles in your digestive tract that helps propel food along. These waves are regulated by your pelvic floor muscles, which control the opening and closing of your bowel. When your pelvic floor muscles relax, the muscles in your rectum contract to push stool out of your body. When your pelvic floor muscles contract, they close off the rectum to prevent stool from escaping until you're ready to have a bowel movement. Unfortunately, when your pelvic floor muscles aren't functioning properly, they can't regulate peristalsis effectively. This can lead to constipation, incomplete evacuation, and other bowel dysfunction. Luckily, pelvic floor physical therapy can help regulate peristalsis and promote healthy bowel movements. Pelvic floor therapists can provide you with exercises and techniques for your pelvic floor muscles, improve your bowel function, and help you regain control over your digestive health. What's Normal? When it comes to bowel movements, it's important to understand what's considered normal and what's not. Many people believe that having a bowel movement every day is a requirement for good health, but this is simply not the case. In fact, the goal is to have a bowel movement at least once every 24 hours, with a range of 12 hours on either side. This means that if you go twice a day, that's great, and if you go once every day and a half to two days, that's also fine. However, if you find yourself only having a bowel movement once every 4-5 days, it is definitely not normal and can negatively impact your digestion, nutrition absorption, and elimination moving forward. When you feel the urge to go, you should be able to wait around 20 minutes before going to the restroom without any accidents or close calls. You should relax your body, open your pelvic floor muscles, and allow your body to naturally expel the stool without force. If you are straining, pushing, or holding your breath to bear down, something is not right. A bowel movement should not be painful, and you should not experience bleeding, cracking, or hemorrhoids. How Many Times Should You Wipe? After your bowel movement is complete, your pelvic floor should close naturally, and you should only need to wipe 3-4 times. If you find yourself wiping excessively or needing to continuously wipe, it may be a sign of a pelvic floor dysfunction, such as an improperly closing sphincter. Not only can excessive wiping be uncomfortable and time-consuming, but it can also lead to skin irritation and other unwanted health issues. The Skinny on Gas Embarrassing gas accidents can be more than just an inconvenience. If you're struggling to control your gas, you're not alone. While it's normal to pass gas, it should be something that you can hold back and only release when you want to. It shouldn't slip out when you're sitting, standing, or exercising. What Should Poop Look Like? It's important to pay attention to the appearance of your stool as it can provide clues about your digestive health. Healthy poop should be smooth and snake-like in shape, with a medium-brown color, a type 4 on the Bristol Stool Chart. Factors such as your diet, hydration level, and medication use can impact stool consistency and color. Moreover, your pelvic floor muscles play a crucial role in bowel function. They should be able to accommodate all types of stool, whether it's small or large, hard or watery. The mu Image Credit : https://khealth.com/learn/bowel-movement/bristol-stool-chart/ In conclusion, understanding what is normal for your bowel movements is crucial to maintaining good health. If you are experiencing discomfort, irregularity, or pain with bowel movements, don't hesitate to seek help. A pelvic floor physical therapist can help you understand what is normal and work with you to promote healthy bowel function.
We'll be diving deeper into a range of bowel movement topics in our upcoming blog posts, including the skinny on constipation, the truth about laxatives and stool softeners, and our favorite tips and tricks for regulating your bowels. Be sure to stay tuned for more valuable insights and information. Sexual health is a fundamental part of our overall health and well-being. That being said, the topic of sexual health is often shrouded in myths, misinformation, and stigma. Lack of information and misconceptions around sex oftentimes cause people to miss out on the joy and pleasure that sex can and should bring. The good news is that you don't have to suffer in silence. Take the first step to taking back control of your sexual health by attending our FREE, empowering, and informative mini workshop titled "The Real Talk: Busting Myths and Improving Sexual Health". This workshop is designed to provide you with accurate information, practical tips, and resources to help you enjoy a healthy, safe, and fulfilling sex life. The workshop is open to everyone, and you are encouraged to come as you are. You do not have to be an expert in sexual health or have any prior knowledge of the subject to attend. The workshop is tailored to suit everyone's needs, and you are welcome to ask any questions you may have.
During the workshop, you will learn about what's normal, what's not, and when to seek help. You will discover practical tips on how to advocate for yourself and communicate with your partner to ensure a safe and enjoyable sexual experience. Additionally, the workshop will also cover ways to address and alleviate sexual stigmas and shame, which can be a significant barrier to discussing sexual health. The goal of the workshop is to provide you with accurate and helpful information that will empower you to make informed decisions about your sexual health. The workshop will be led by experienced sexual health professionals from several different organizations who will answer your questions and provide you with practical tips to improve your overall sexual health. Restoration Health Collective, STAR (Sexual Trauma Awareness and Response Center), and Sofia will all be in attendance and have representatives present to answer any and all questions. By attending the workshop, you will have the opportunity to connect with others who may be going through similar experiences as you. You will also receive FREE giveaways and refreshments to make your experience more enjoyable. Don't let myths, stigmas, and lack of information about sexual health hold you back any longer. Join us for this free, empowering, and informative mini workshop on sexual health, and take a step towards a healthy, safe, and fulfilling sexual life. WHERE : The Red Shoes on Government , 2303 Government St, Baton Rouge, LA 70806 WHEN: March 1. 2023 @ 5:00 P.M. The media, whether it be movies, television, or porn, loves to portray an orgasm as this explosive release that happens so easily and with very minimal effort. The reality is that it isn't that easy for the majority of the population, in fact, research tells us that 30% of women "rarely or never" orgasm during vaginal intercourse and between 5-10% of people who have a vulva experience anorgasmia at some point in their lives. Our patients come to us telling us they feel like the "fireworks" they once experienced are just a dull sparkle now, some tell us they've never reached an orgasm and don't even know what it would feel like if they did have one, and some patients tell us that they can only achieve an orgasm when they use a certain toy, alone, or with a certain partner. This leaves so many people feeling hopeless and full of self-doubt that they can't preform for themselves or for their partners. If this is you, don't give up hope! With time and knowledge you can get back to feeling like yourself again & take back control of your sex life, continue reading to learn more. What Is Anorgasmia? Anorgasmia is described by the Mayo Clinic as "delayed, infrequent, or absent orgasms - or significantly less-intense orgasms — after sexual arousal and adequate sexual stimulation". It's important to remember that orgasms vary drastically from one person to another, no two are alike, so make sure you take that into account. Compare against yourself, not against other people. It's also necessary to note that there can be a myriad of factors that can contribute to your ability to perform sexually aside including alcohol or drug use, certain medications like SSRIs, and various psychological factors like your perception of yourself, body image issues, and low self esteem. Anorgasmia can be categorized into several different categories: primary, secondary, and situational and they all manifest themselves in different ways. Primary Anorgasmia is a condition in which a person has never had an orgasm in any way, whether that be via penetrative intercourse, oral, manual stimulation or masturbation and regardless whether it's solo or with a partner. Secondary Anorgasmia is defined as a condition in which a person has achieved orgasms in the past but no longer can, or is unhappy with the amount of time it now takes them to reach an orgasm, or is frustrated with the sensation of orgasms now compared to in the past (ie. Used to feel fireworks, now feels like a dull sparkle). Situational Anorgasmia is when a person can only reach an orgasm in certain situations with specific types of stimulation or specific partners. How Do The Pelvic Floor Muscles Play a Part? We learned in previous blog posts that the pelvic floor is a group of muscles that form a sling-like structure at the base of the pelvis, these muscles go from front to back and from side to and that they play a crucial role in supporting the pelvic organs as well as inhibiting sexual function. The superficial pelvic floor muscles function to help people achieve an erection, ejaculate, and orgasm. I think My Pelvic Floor is Affecting My Sexual Function, What Now? If any of these symptoms or sensations speak to you, don't panic, you're not alone and you can overcome this. We understand that sexual health and being content and happy with your sex life plays a huge role in many people's mental health & the strength of their relationships. One excellent way to improve sexual function, regain your confidence, and take back your sex life is through Pelvic Floor Physical Therapy. Pelvic Floor PT has been shown time and time again to improve sexual function in both men and women, whether that be lack of orgasm, pain with intercourse, or a combination of the two. At Restoration Health Collective our team of pelvic floor specialists will create a personalized treatment plan specifically for your needs and goals. You'll receive one-on-one care with a physical therapist who is dedicated to helping you reach your goals and take back your confidence once again. Have More Questions About How Pelvic Floor PT Can Help You Regain Your Sexual Function?
Download our FREE Sexual Health e-Book by clicking HERE |
















 RSS Feed
RSS Feed